There’s a new incident every day.
Most recently, it was three Black football players being shot to death following a school field trip. Right before that, there was the video of a white teacher telling Black students that his race is “the superior one.” Earlier this year, a different football team’s season was suspended after reports of alleged “disturbing” racist remarks in a group chat. And there was the other football season that was canceled after students participated in a “mock slave trade” — which somehow isn’t uncommon, with at least three other instances of it in the last year.
But these are only the ones that are filmed. The ones that gain traction online.
On top of these recorded incidents, Black students face racism every day. And on top of that, there’s still residual trauma from the pandemic. These combined forces are wreaking havoc on students’ mental health and, subsequently, their ability to perform in school.
“We aren’t doing a good job,” says Lishaun Francis, the director of behavioral health at the California-based organization Children Now. “Mental health has become a big thing in the last two years for folks, but the reality is, as a nation, we have under-invested in mental health for decades.”
The cracks are beginning to show. COVID-19 shone the light on the limitations of our public health system.
“We added on more emotional distress,” Francis says, “and the cracks in the foundation are really showing that it has problems.”
A Volcano Waiting to Erupt
Unresolved or unaddressed emotional issues impact the way a student performs “in every way imaginable,” Francis says.
Black students, especially, may be having different experiences than their classmates, says Dr. Janice Beal, who owns a private practice in Houston and partners with The Steve Fund as a mental health expert. Whether it’s a home environment, difficulty processing trauma exposure, or specific discrimination, like anxiety over the fear of being stopped by police, there’s an impact if these feelings build up and go unresolved.
Beal equated these feelings to lava in a volcano: They stay at the bottom for a long time and pressure starts to build.
“Now what may happen is it may be buried, and no one is talking about it, and no one’s addressing it,” Beal says. “At some point, it explodes and exposes things that may not be associated with what their original trauma was, but they may have kept.”
This is especially true among communities of color, who are less likely to seek mental health treatment. But the pandemic helped to shift that.
“Everybody now understands and is willing to have that conversation,” Beal says. “More parents are more open to talking to their children about mental health; however, there’s still a major stigma within our communities.”
In its 2022 report card, Children Now graded California with a D+ for mental health. Despite the state having a progressive reputation, the report card said families are often only able to find mental health services “due to perseverance, privilege, and luck rather than a comprehensive system.” And, it says, more focus needs to go into increasing culturally competent providers and boosting mental health first aid training for adults who work with kids.
The mental well-being of California youth declined dramatically during the pandemic, according to the report card. Prior to the pandemic, 68% of students rated their mental wellness between 7-10 on a 10-point scale, compared to only 39% of youth post-pandemic. There has also been a dramatic increase in suicide rates among Black youth, which the report attributes to “exposure to overt and systemic racism and lack of treatment for depression.”
And the Children’s Hospital Association said that in 2021, compared to five years earlier in 2016, children’s hospitals saw a 153% increase in visits to emergency departments for kids ages 5-18 attempting suicide and other self-injuries. There was also an increase in kids in that age group boarding in hospitals for mental health reasons, up 84% since the pandemic, and 75% of hospitals are reporting longer stays.
The problem is that it can be difficult to identify. Mental health and emotional wellness show up differently in everyone — whether it’s the obvious “problem child” who is constantly misbehaving and getting low grades, or the people pleaser who is a straight-A student and never wants to disappoint anyone.
“You often see this in kids who experienced trauma, that they are so concerned about doing everything right,” Francis says. “But the reality is it shows up in kids very differently, and we only really recognize and acknowledge the kids who have low grades and act out because it’s easier to identify.”
In-School Resources and Their Limitations
The availability and types of resources offered in schools depend on where you are — both in terms of state and district — because schools are run by “local and localized decisions,” Francis says.
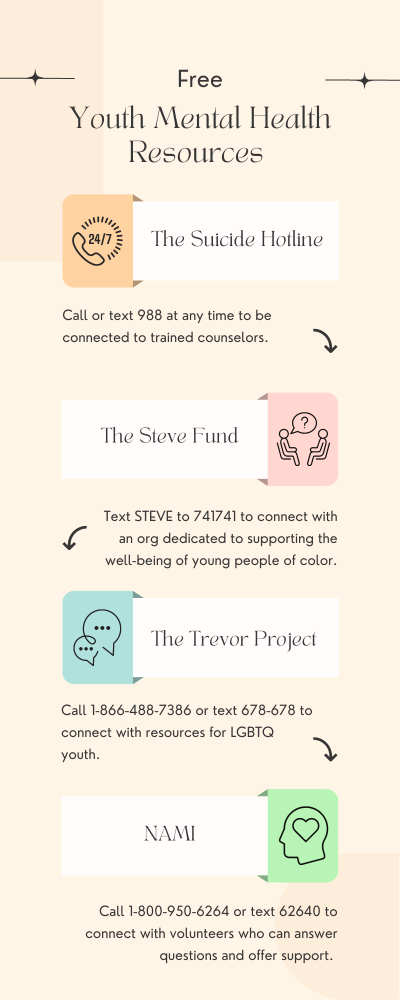
To help fulfill the in-school resources, schools often partner with outside programs. For example, schools will provide a list of online resources that students can turn to for help, like NAMI and The Trevor Project, and advertise the suicide prevention hotline, which is now 988.
During the pandemic, when demand for mental health services skyrocketed, many states started creating websites to streamline resources “to educate families about resources that are available,” Francis says. “We were really happy to see that because there’s so much information out there, people don’t know where to look.”
And some schools and turning to telehealth, which allows students to access mental health resources during the day even though the help isn’t in the building.
“The partnerships are developing in order to be able to meet some of the needs the students have,” Beal says. “Community partnerships are so important.”
But there are often limitations to school-based resources — even when it comes to websites.
For one, websites alone bring access issues. Those living in rural communities often lack regular or private access to strong internet connections.
The National Association of School Psychologists recommends the ratio of students to psychologists is 500 to 1, but the current ratio is about 1,162 to 1. So while affluent students may be able to afford private mental health professionals, students who can’t — or whose parents won’t support them getting help — are stuck fighting for access to an already overwhelmed system in the school.
So, while learning about mental health issues and disorders is free on a website, what isn’t free is having to pay for the services. This is a different set of limitations on access.
“Black people, in particular, feel like there is a dearth of providers who can respond to their specific cultural needs, even though there’s a lot of information online about black mental health,” Francis says.
When it comes to addressing students’ mental health needs, schools often operate under the notion that there isn’t a problem because they don’t see one. But it’s important to do the work instead of the clean up, says Ashanti Branch, the founder and executive director of the Oakland-based Ever Forward Club.
But what educators need to realize is that, during virtual learning, there were students who spent 24 hours a day without love for an entire year — and some dealing with much worse.
“I don’t know that teachers got a whole lot of specialized training — definitely not dealing with returning from a pandemic — because most of those teachers today, most of them never lived through one,” Branch says. “We find that they’re not getting the training, the support, the mental health and mental wellness care that they desperately need.”
The Staffing Shortage Extends to Mental Health Professionals
As schools across the country face teacher shortages, those aren’t the only positions that need to be filled. Even prior to the pandemic, school counselors and psychologists were hard to come by in majority non-white schools — especially Black mental health professionals.
“We are still suffering from the effects of not having enough adults in the room to take care of children,” Francis says.
Now, there are 5.4 million, or 12%, public school students attending districts that don’t have psychologists and half a million, or 1%, in schools without counselors, according to an Education Week analysis. And, of course, the shortages continue to be felt in certain districts and schools more than others.
The analysis broke it down further, finding that districts that have higher percentages of white students are more likely to meet the recommended mental health staff-to-student ratios. For example, in districts that were majority non-white, only 6% met the ratio for school psychologists, compared to more than 9% of majority-white districts. And, along those lines, 10% of majority non-white districts met the recommended counselor-to-student ratio, compared to 16% of majority-white districts.
But throwing money at the problem won’t solve it. It matters who the mental health professionals are and what their backgrounds are — especially whether their training focused on kids.
“We need to increase our pipeline, we need to increase our workforce that focuses on children,” Francis says. “Otherwise, we’ll just have a bunch of adults that were trained to work with other adults.”
What Do We Do?
In California, there aren’t any large-scale training efforts to help teachers better identify and address mental health problems in students. There was a push in many counties, Francis says, to train county workers, teachers, and staff on what emotional distress looks like through various programs, but it never reached all the schools in the state.
“We have never done a good job scaling anything, which means that only some communities have gotten something,” Francis says. “Oftentimes, it was those communities who had the staff where the teachers and the advocates knew enough to ask for it.”
But part of the problem with additional trainings — or more events added to a tightly packed calendar — is it overwhelms teachers, who have their own mental health to address.
“The fact of the matter is our adults aren’t okay,” Francis says. “Not enough attention is being paid to that, and we’ve kind of missed the mark, and we aren’t recognizing it as much.”
But teachers are trying — both by seeking out information to better help their students and through new practices. One of the initiatives Beal introduced is the morning check-in. And it only takes a few minutes.
“You can notice if there’s a difference based on how the student responded to that question,” Beal says. “Then you can look at your class and say she’s not acting her normal self, she feels a little quiet, and you may want to give her the opportunity to go and talk to the counselor if she wants to.”
And Beal also helped initiate peer counselors, who were trained to help inform their fellow students about mental health and best practices. This, above all, gives Beal hope: This generation is willing to talk about mental health.
“The culture is changing, as far as Black students,” Beal says. “We just need that little bit of help and trust factors.”