By Rae Ellen Bichell, KHN
Two months before the Super Bowl, the omicron surge was decimating NFL rosters as players tested positive for covid-19. In mid-December, the NFL postponed a game between the Los Angeles Rams and the Seattle Seahawks because the Rams, who would go on to win the Super Bowl, had 29 players out with covid.
The number of NFL employees testing positive per week in December went from about 30 to about 300, most of them players who would have to sit out of practices and games. The new variant “hit us like a ton of bricks,” said Dr. Allen Sills, chief medical officer for the NFL.
Dr. Thom Mayer, medical director for the NFL Players Association, said the disruption brought to the fore a big question: If a player was vaccinated and recovering from covid but still tested positive, were there conditions that might make it “reasonable to return them [to the field] and safe to do so?”
The NFL and the players association determined there were. The same week the NFL postponed the Rams-Seahawks game, the league made a small but meaningful change to its rules for allowing players to return after testing positive for covid, one that hinges on an arcane measurement called a cycle threshold, or Ct value.
A Ct value indicates how hard it was for the test to detect the virus and therefore how much or how little of the virus was present in a person’s swab sample. Now, players could return either hewing to the previous standard of two negative PCR tests, or with two PCR results that Mayer described as “faintly positive” — with a cycle threshold of 35 or higher. They could also mix and match the two options.
The change essentially redefined what counted as negative to get players back in the game sooner. By doing so, the NFL stepped into a covid-testing gray area that’s been debated by public health professionals for the entire pandemic: how to determine when someone is no longer infectious with covid.
The core issue is there’s no good way to know whether a person is infectious. Antigen tests, the kind people can do at home and register results within a matter of minutes, are too “cold,” prone to missing people who are in the first few days of their infection. PCR tests are too “hot,” so sensitive they can continue to register someone as positive after an infection has cleared.
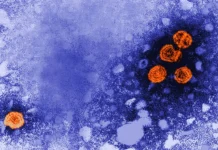
But PCR tests often come with more information than just “positive” or “negative”: They can also report how many times the machine had to copy the genetic material of the virus in the sample before it yielded enough to actually see. More cycles typically means the sample didn’t have much virus to work with; fewer cycles means there was enough virus around in the sample that it was easy to detect.
In defining a Ct value cutoff for PCR tests, which some researchers support, the NFL was essentially seeking a medium ground by cooling off the too-hot test. The logic goes that higher Ct values means less virus is present in the sample, so there’s a smaller chance the person who provided it can infect another person.
“We’re looking for the sweet spot,” Sills said. “We don’t want to return somebody too early who’s infectious. We also don’t want to keep someone out of an environment when they aren’t sick and are no longer infectious.”
Sills recently co-authored a Centers for Disease Control and Prevention article that focused on NFL employees who tested positive for covid during the same week in mid-December. It showed that among 173 frequently tested, fully vaccinated NFL employees, about 70% were able to return to work before 10 days of isolation was up, under the new testing protocols.
The problem is that using Ct values to determine infectiousness isn’t yet validated by the FDA — PCR tests have been given emergency use authorization for the sole purpose of determining whether someone is “positive” or “negative,” not for determining how positive they might be.
The CDC has said “a high Ct value can easily result from factors not related to the amount of virus in the specimen” and that Ct values “should not be used to determine an individual’s viral load, how infectious an individual person may be, or when an individual person can be released from isolation.”
The NFL was willing to go there because its employees were overwhelmingly vaccinated, its covid cases were mostly mild, and internal data from previous variants suggested people with high Ct values weren’t capable of spreading the virus, Sills said. And, as Mayer pointed out, “if the games don’t get played, the players don’t get paid.”
Some researchers draw a line at a Ct value of 30, assuming that everyone with a test result below that number is likely infectious and everyone above it likely isn’t. But other researchers were able to culture live virus from people with high Ct values, which is considered proof that those people were infectious. And for the past two years, laboratory medicine professionals have cautioned against using Ct values for making decisions about individual care, including in determining who is infectious.
“That’s such a gray area right now, in terms of what exactly defines when you’re infectious and when you’re not,” said Dr. Stephen Master, president of the American Association for Clinical Chemistry, which put out a statement over the summer saying that Ct values shouldn’t be used and published a blog post in December called “How to Say No to Reporting Ct Values.”
Master said it takes a lot of work to make sure that such results match some sort of usable standard and the fact one doesn’t exist is “an underrecognized problem” even among top doctors. “Unless you’ve got the reference method and the reference standard, it’s hard to know what’s real.”
Scientists working on developing a reference standard sent the same virus samples to more than 300 labs and found that what looked like a Ct value of 17 in one lab was a Ct value of 27 in another.
In concluding that no one whose test had a Ct value of 35 or over could transmit the virus, the NFL’s Sills relied on data from the league’s 32 teams. And the NFL got around one variability obstacle by requiring that all the PCR tests be done on the same lab equipment — Roche’s cobas analyzer — and by certain laboratories.
Even then, said Jim Huggett, a molecular biologist with the University of Surrey in the United Kingdom who has studied variability in Ct values in labs internationally, two labs using the same equipment could get different results, meaning the same person on the same day could get different Ct values. As the American Association for Clinical Chemistry pointed out, even super-precise labs can’t control outside factors like whether the person blew their nose before swabbing or how long the sample sat around before it was analyzed — both of which can affect Ct values.
Dr. Rosemary She, a pathologist with the University of Southern California’s Keck School of Medicine and the director of microbiology at Keck Medical Center, said a high Ct value can sometimes correspond to nothing more than poor swabbing.
In 2020, she co-authored a letter while representing the College of American Pathologists that cautioned against using Ct values to determine what might be going on in any one person’s body. Among the hospitalized patients she tests, a Ct value as high as 40 can mean either “the tail end of an infection” or just “bad sampling,” she said.
Dr. Robby Sikka, chair of the COVID Sports and Society Working Group — which advises tech companies, sports leagues, and Broadway on their covid responses — is more optimistic about the utility of Ct values. He said data from athletic and corporate settings show a lot of promise. For example, his small, preliminary study looking at 37 people in a highly vaccinated workplace showed that people who returned after at least five days of isolation, followed by two PCR tests with Ct values of 30 or higher, didn’t transmit the virus to any colleagues.
At the community level, James Hay, an infectious disease epidemiologist at the Harvard T.H. Chan School of Public Health, published a study in the journal Science that showed that just 30 positive PCR tests provide enough information, when Ct values are taken into account, to show whether an outbreak is growing or declining.
Researchers in South Africa and the U.K. are studying Ct values to track the direction that outbreaks go, and scientists in Hong Kong say Ct values provide a quicker way to know what’s going on than looking at case counts — and potentially quicker than tracking the coronavirus in communities through wastewater samples.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.