By Jazelle Hunt
NNPA Washington Correspondent
WASHINGTON (NNPA) – Rae Lewis Thornton likes to sneak in a tranquil tea time between expanding her brand and the 16 pills she has to take each day. But that’s nothing compared to the 21 pills she was taking in her darkest days of battling full-blown AIDS.
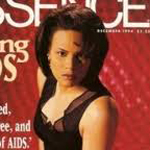
Thornton was diagnosed with HIV at 23 years old after attempting to donate blood. The following year she shared her story and made the cover of Essence magazine, instantly becoming toe face of HIV/AIDS for young, successful, heterosexual Black women, catapulting herself into a life of activism and ministry. Today, she continues to minister, teach, and welcome the world into her life through her award-winning syndicated blog, Diva Living with AIDS.
And she certainly is living. Now 51 years old, Thornton is an Emmy-Award winner, author, life coach and motivational speaker, jewelry designer, and avid reader.
“One thing I’ve done is live incredibly well with this disease,” says Thornton, who lives in Chicago. “But don’t confuse my HIV now with how it used to be. Now, they can keep you here and you can live a long life, but it is a very hard life.”
As of 2010, the HIV/AIDS mortality rate is 2.7 (per 100,000), down from 8.3 in 1990. Thanks to advances in research, treatment, and global management, HIV-positive people are living longer, better lives.
“It’s a mixed bag. We are still saddened by every new infection, and they’re still happening so rapidly,” says Adam Tenner, executive director of D.C.-based nonprofit, Metro Teen AIDS. “But it’s not like the old days, when we were burying people very quickly after diagnosis. We spend so much time looking at what’s broken, we don’t often look at what’s working.”
And there is a lot that is working. In D.C. for example, where the infamous infection rate has been compared to that of developing nations, the Department of Health is touting a 50 percent decline in new cases over the past four years, thanks to a battery of free services and community awareness campaigns. Nationally, the rate of infection for Black women is on the decline. Globally, the rate of new infections has dropped 33 percent since 2001.
“Things in 2013 are very, very, very different than it was in 1982, or 1992, or even 2002,” says Phill Wilson, founder and director of the Black AIDS Institute. “The treatments available today are better, faster, more effective, and less toxic than ever before.”
It’s not an overstatement to call the first generation of antiretrovirals toxic. HIV/AIDS medications are designed to block the enzymes that allow the virus to replicate; but in the 1990s, the drugs blocked both the virus and the body’s ability to generate healthy cells, thus crippling tissues and organs. Side effects included nausea, diarrhea, concentrated fatty deposits in some areas and natural-fat deterioration in others, kidney disease, hepatitis, bone loss, and even nerve damage.
People had to take a handful of these pills, several times daily. And usually, doctors wouldn’t start prescribing these pills until after the virus’ symptoms became dire.
Today, someone who’s diagnosed early and begins treatment immediately might take three pills a few times a day, with few, if any, dietary restrictions, and with mild side effects.
Wilson has been living with HIV for 35 years.
“I live an active life. I work, some would say too hard. I run, hike, scuba dive, white water raft – none of that would be possible without treatment,” he says. “And I’m not special. It’s not like I have secret access to something others don’t have access to.”
Improved treatment has also unexpectedly given rise to the development of preventative measures beyond the condom.
As Tenner, of Metro Teen AIDS explains, “We know that if we can get people on anti-virals early it improves their outcomes, but it also makes them less likely to transmit to others. You literally become less infectious. So what’s coming down the pike is how HIV negative people can protect themselves. We’re starting to put more tools in the box for people at higher risk of contracting HIV.”
He’s referring to pre-exposure prophylaxis (PrEP) treatments, which greatly reduce the chance of infection even if someone comes in direct contact with a pathogen (such as the HIV virus). It’s an old medical concept, but last year the drug Truvada became the first FDA-approved pill to protect against HIV. It was already in use as a treatment to lower the viral count in HIV-positive patients.
It’s still early, but those in the know are optimistic about Truvada’s potency as a PrEP pill.
“Every infection involves a -negative person and a –positive person, and now we have an answer for both sides of the equation,” Wilson says. “If we can get someone to a suppressed viral load, that reduces their ability to transmit by 96 percent. Condoms offer 70-percent protection, but if you’re on a pre-exposure prophylaxis and you do get exposed, you can reduce contracting HIV by 92 percent.”
The Affordable Care Act will have also have a major impact on the future HIV/AIDS in the United States.
Wilson says, “For people living with HIV, the Affordable Care Act will have a positive impact on all 1.1 million of us. It’s a game-changer in the world of HIV.”
HIV/AIDS is a difficult, expensive illness, and without insurance it’s hard to fight. Young people with HIV/AIDS have usually been ineligible for insurance for their pre-existing condition. If a person living with HIV did manage to get insurance, their provider could drop them if their medical bills got too expensive. If that person managed to keep their insurance and pay their premiums each month, they could still be denied coverage if their bills breach the annual or lifetime medical cost cap.
The ACA outlaws all of these insurance practices.
On November 21, HIV-positive Americans also gained another layer of health care access when President Obama signed the HIV Organ Policy Equity Act (HOPE) into law. First introduced in February, the HOPE Act revises current laws to allow the Organ Procurement and Transplantation Network to set up regulations for acquiring, transporting, and transplanting organs infected with HIV for HIV-positive patients who need them. The bill also decriminalizes organ donation for HIV-positive Americans (as long as it is done under these regulations), and calls for annual research and revisions for these guidelines.
Although much progress has been made, HIV/AIDS is still an epidemic.
The infection rate among young men of all races who have sex with men (gay, bisexual, or MSM) is still high, with 28,500 new diagnoses in 2010. One in five people living with HIV are unaware of their status. Advocates and organizers say the stigma surrounding HIV still not only prevents people from getting tested, but also from sharing their positive status with loved ones and sexual partners.
In addition, the disease is no longer “the sexy health topic to talk about,” according to Thornton.
Still, there is progress. The future of HIV/AIDS lies in developing PrEP methods; in widespread, early diagnosis and treatment; and in providing support and resources for those who are diagnosed with or affected by the virus.
Wilson says we all have a role to play in eradicating HIV/AIDS, and that community support for the organizations leading the fight is crucial. Thornton agrees, citing the support of the Black church as one of the most encouraging things she’s seen in her travels.
“We won’t be able to end the epidemic if we don’t do the right thing. Now is the time to renew our dedication to fighting HIV/AIDS, because we now have the pathways to get there,” Wilson says. “And for the Black community, we need to stay involved to make sure we aren’t left behind. It would be tragic to lose this opportunity.”